

xxxxxThe English surgeon Joseph Lister is regarded as the founder of antiseptic medicine. In 1865, influenced by the germ theory put forward by Louis Pasteur, he introduced strict rules of hygiene in the operating theatre, and applied carbolic acid, a powerful disinfectant, to wounds and bandages in order to reduce the possibility of infection after surgery. His methods, introduced while working at Glasgow Royal Infirmary in the 1860s, proved highly successful, and reduced the number of deaths from 45 to 15 percent in a matter of two years. By 1880 his methods had won approval and were in wide use. He also worked in the clinical surgeries at Edinburgh Royal Infirmary and King’s College Hospital, London, where he contributed to the advance of health education. For his services to medicine he was made a baronet in 1883, and raised to the peerage in 1897. He was also president of the Royal Society for five years, and in 1902 was appointed one of the original twelve members of the Order of Merit. His method of antisepsis, together with the advent of anaesthesia, mark the beginning of modern surgery.
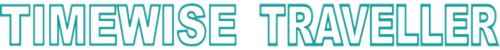
JOSEPH LISTER 1827 - 1912 (G4, W4, Va, Vb, Vc, E7, G5)
Acknowledgements
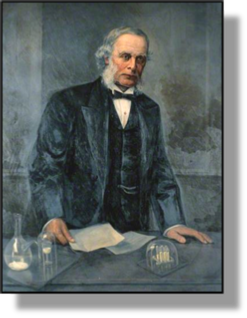
Lister: by the English artist Harry Herman Salomon (1860-1936) – Wellcome Library, London. Operation: date and artist unknown. Bergmann: 1888, artist unknown, contained in Kaiser Fredrich III, Liberal Hope of Germany by the German historian Franz Herre (born 1926). Charcot: by the French photographer and filmmaker Eugène Pirou (1841-1909). Villemin: date and artist unknown. Pasteur: date and artist unknown – Musée Pasteur, Paris.
 xxxxxIn 1865 the English surgeon Joseph Lister, influenced by Louis Pasteur’s work on bacteria, became the founder of antiseptc medicine. By introducing strict rules of hygiene in the operating theatre and applying carbolic acid, a powerful disinfectant, to reduce the possibility of sepsis (infection) after surgery, he achieved a two-third reduction in the number of patients dying from infected wounds. This method of antisepsis, together with the advent of anesthesia, mark the beginning of modern surgery.
xxxxxIn 1865 the English surgeon Joseph Lister, influenced by Louis Pasteur’s work on bacteria, became the founder of antiseptc medicine. By introducing strict rules of hygiene in the operating theatre and applying carbolic acid, a powerful disinfectant, to reduce the possibility of sepsis (infection) after surgery, he achieved a two-third reduction in the number of patients dying from infected wounds. This method of antisepsis, together with the advent of anesthesia, mark the beginning of modern surgery.
xxxxxListerxwas born in Upton, Essex, and after attending two Quaker institutions, he studied medicine at University College, London, and then Edinburgh University, where he worked as assistant to the well-known Scottish surgeon James Syme (1799-1870) and joined the staff of the Edinburgh Royal Infirmary. He was appointed surgeon at Glasgow Royal Infirmary in 1861, and it was there that he did his pioneering work in antisepsis. Put in charge of a new surgery unit specifically designed to reduce the number of deaths from gangrene and other infections - then running at about 45 percent - he failed to make any appreciable improvement over the next four years, despite every effort to keep the wards, theatre and the surgical instruments thoroughly clean.
xxxxxThe break through came in 1865. Dissatisfied with the current belief that infection was caused by bad (polluted) air, he came to see Louis Pasteur’s germ theory as more in line with his own idea that sepsis was caused by some form of dust. With this in mind he began using carbolic acid not only to clean the operating theatre, the wards and the surgical instruments, but also to provide a barrier between the wound and the germ-containing atmosphere. Following an operation, bandages and ligatures were dipped in the acid, thereby preventing bacteria from entering into an open wound. The results were highly successful. In 1867 Lister was able to announce that all his wards had been free from sepsis for nine months, and that the mortality rate had fallen from 45 to 15 percent.
 xxxxxIn 1869 Lister was appointed to the chair of Clinical Surgery at Edinburgh, succeeding his former tutor James Syme. He continued his antisepsis work, aided by the advances made in this direction by German surgeons during the Franco-Prussian War. As a result his department attracted a large number of medical students, and hundreds attended his public lectures. In 1875 he made a successful tour of the leading surgical centres in Germany, but his visit to the United States was not so well received. In America, in fact, and in Britain too, there was still some scepticism over the germ theory, and it was not until 1877, when he took up the chair of Clinical Surgery at King’s College Hospital, London, that he was able to convince the doubters. It was then that he carried out the first successful operation on a fractured kneecap - an operation that had nearly always led to infection and death - and clearly proved the value of his antisepsis precautions. By the early 1880s his methods had become widely accepted and were in common use, though, as the illustration above shows, surgeons still used their normal clothing, and face masks and rubber gloves were yet to come.
xxxxxIn 1869 Lister was appointed to the chair of Clinical Surgery at Edinburgh, succeeding his former tutor James Syme. He continued his antisepsis work, aided by the advances made in this direction by German surgeons during the Franco-Prussian War. As a result his department attracted a large number of medical students, and hundreds attended his public lectures. In 1875 he made a successful tour of the leading surgical centres in Germany, but his visit to the United States was not so well received. In America, in fact, and in Britain too, there was still some scepticism over the germ theory, and it was not until 1877, when he took up the chair of Clinical Surgery at King’s College Hospital, London, that he was able to convince the doubters. It was then that he carried out the first successful operation on a fractured kneecap - an operation that had nearly always led to infection and death - and clearly proved the value of his antisepsis precautions. By the early 1880s his methods had become widely accepted and were in common use, though, as the illustration above shows, surgeons still used their normal clothing, and face masks and rubber gloves were yet to come.
xxxxxApart from his clinical work, Lister showed an interest in hygiene in hospitals, the transport of the sick and wounded, and health education in general. In 1891, while working in London, he was appointed to the chair of the British Institute of Preventive Medicine, later renamed the Lister Institute in his honour. In recognition of the advances he made in medical knowledge, he was made a baronet in 1883 and raised to the peerage in 1897. He also served as president of the Royal Society from 1895 to 1900, and in 1902 was appointed one of the original twelve members of the Order of Merit. A quiet, unassuming man, he was dedicated towards his work and modest about his achievements.
xxxxxListerxwrote many papers to professional journals, but he did not write a book. However, the English surgeon William Cheyne (1852-1932) who worked with him at King’s College Hospital and was a staunch supporter of his new antiseptic methods, published Antiseptic Surgery: Its Principles, Practice, History and Results in 1882, and three years later produced Lister and His Achievements.
xxxxxIncidentally, carbolic acid, sometimes referred to as “phenol”, was a chemical that was being used at this time to combat foul-smelling sewers. ……
xxxxx……xLaterxin his career Lister used steam to sterilize surgical instruments, a method introduced by the German surgeon Ernst von Bergmann (1836-1907) in 1886. He served in both the Austro-Prussian and Franco-Prussian Wars and became a specialist in the treatment of brain disorders and the nervous system. ……
Xxxxx……xLister was a great admirer of the Hungarian physician Ignaz Semmelweiss. He introduced cleaning methods while working in Vienna in the 1840s - including the washing of hands - and this brought about a marked reduction in the number of cases of puerperal fever. ……
xxxxx…… Lister, along with John Hunter, are the only two British surgeons who have a public monument in London to commemorate their contribution to medicine. Lister’s statue stands in Portland Place, and there is another of him in Kelvingrove Park, Glasgow, the city closely associated with his pioneering work.

xxxxxA number of notable advances were made in medical knowledge at this time. ThexFrench physiologist Claude Bernard (1813-1878), founder of experimental medicine, is remembered above all for his thorough research into the digestive system. His work, which included the discovery of the vasomotor nerves and additional functions of the liver, was summed up in his The Introduction to the Study of Experimental Medicine, published in 1865. Meanwhile his fellow countryman, the neurologist Jean-Martin Charcot (1825-1893) (illustrated) made a special study of senile diseases, was the first to name and describe multiple sclerosis, and in the early 1860s added further to the symptoms of Parkinson’s disease. He is best remembered today for giving greater credence to hypnosis, used to good effect in his study of hysteria. Among his students was the famous Austrian psychoanalyst Sigmund Freud (1856-1939).
xxxxxAnd two doctors made important discoveries in tropical medicine. ThexNorwegian physician Armauer Hansen (1841-1912), a firm supporter of Darwin’s theory of evolution, discovered the leprosy bacillus in 1873. (Leprosy is sometimes known as Hansen’s disease). Sevenxyears later the French physician  Alphonse Laveran (1845-1922) examined blood samples from patients suffering from malaria and discovered the parasites which cause this disease.
Alphonse Laveran (1845-1922) examined blood samples from patients suffering from malaria and discovered the parasites which cause this disease.
xxxxxInx1867, after lengthy research, the French physicist Jean-Antoine Villemin (1827-1892) (illustrated) made known that tuberculosis was an infectious disease, but at that time it was generally considered that the disease was hereditary, and his finding was not widely accepted. It was not, in fact, until the early 1880s that the German bacteriologist Robert Koch isolated the tubercle bacillus and proved him right.

xxxxxLouis Pasteur (1822-95) was an outstanding scientist. His development of the germ theory of disease proved the single and most important contribution to medical science. As we have seen, his study of fermentation in the making of wine, begun in 1858 (Va), introduced the process known as “pasteurisation”, and his experiments to disprove the theory of spontaneous generation (the idea that living organisms, like maggots, could be generated by non-living things) persuaded him that diseases were spread by “germs” contained in particles of dust. He became convinced of this idea when in 1865 he was tasked with saving the French silkworm industry, struck down by a virulent disease. He discovered that this was caused by a tiny parasite, and he stopped the outbreak by destroying all the infected worms, and the leaves they fed off, and re-starting the industry based on healthy worms. His germ theory of disease did not convince all, but by the 1880s many surgeons, like Joseph Lister, were taking antiseptic precautions to stop the spread of disease carried in the atmosphere. By this time Pasteur had turned his attention to preventative medicine. As we shall see, in 1881 (Vc) he employed inoculation to prevent anthrax in sheep and cattle, and then went on to find a vaccine for chicken cholera and rabies in both humans and dogs.
 xxxxxLouis Pasteur (1822-1895) proved to be on of the greatest scientists of all time. His development of the germ theory of disease proved a major break through in the advance of medical science. As we have seen, it was in 1858 (Va), whilst studying the process of wine making, that he recognised that fermentation involved living organisms. He established further that when the liquor turned sour, it was due to the presence of additional, harmful microscopic life. This could be destroyed by a controlled heating process, a method which came to be known as “pasteurisation” and came to be used extensively in the milk industry.
xxxxxLouis Pasteur (1822-1895) proved to be on of the greatest scientists of all time. His development of the germ theory of disease proved a major break through in the advance of medical science. As we have seen, it was in 1858 (Va), whilst studying the process of wine making, that he recognised that fermentation involved living organisms. He established further that when the liquor turned sour, it was due to the presence of additional, harmful microscopic life. This could be destroyed by a controlled heating process, a method which came to be known as “pasteurisation” and came to be used extensively in the milk industry.
xxxxxIn 1860, he took this theory further by proving that a bowl of soup, when open to the air, would become contaminated by tiny living organisms (“germs”) contained in particles of dust. However, once the soup was protected from these dust particles by some kind of filter, it remained unharmed and edible. This not only disproved the theory of spontaneous generation (the idea that living organisms such as maggots were generated from non-living things) but also opened the possibility that diseases were spread from person to person by such means. It was this very suggestion that led the English surgeon Joseph Lister to introduce carbolic acid as a barrier between an open wound and the germ-containing atmosphere.
 xxxxxAn opportunity for Pasteur to learn more about infectious diseases came in 1865 when he was the administrator and director of scientific studies at the École Normale in Paris. It was then that he was commissioned by the government to go to the assistance of the silk industry in southern France. A disease among the silkworms, known as pebrine, had killed off the silkworms in large numbers and put this thriving industry in danger of complete collapse. After microscopic observation of the diseased silkworms, the moths and their eggs, Pasteur proved that the disease was due to a tiny parasite and that apart from being highly contagious, the disease was also hereditary. His solution was to destroy all infested worms and mulberry leaves (on which the worms fed) and re-establish the industry based on healthy worms. By this method the French silk industry, an important part of the country’s economy, was virtually saved from extinction.
xxxxxAn opportunity for Pasteur to learn more about infectious diseases came in 1865 when he was the administrator and director of scientific studies at the École Normale in Paris. It was then that he was commissioned by the government to go to the assistance of the silk industry in southern France. A disease among the silkworms, known as pebrine, had killed off the silkworms in large numbers and put this thriving industry in danger of complete collapse. After microscopic observation of the diseased silkworms, the moths and their eggs, Pasteur proved that the disease was due to a tiny parasite and that apart from being highly contagious, the disease was also hereditary. His solution was to destroy all infested worms and mulberry leaves (on which the worms fed) and re-establish the industry based on healthy worms. By this method the French silk industry, an important part of the country’s economy, was virtually saved from extinction.
xxxxxIt was from this study of the silkworm disease, together with his previous work on fermentation and spontaneous generation, that led to Pasteur’s germ theory of disease, a theory that was the single and most important contribution to medical science and the practice of surgery. It was not universally accepted overnight - sceptics remained for some years - but by the 1880s the majority of medical scientists had been convinced, and medical establishments were taking many of the antiseptic precautions necessary to prevent the spread of infection. By this time Pasteur had turned his attention to preventative medicine. As we shall see, in 1881 (Vc) he employed inoculation to prevent anthrax in sheep and cattle, and then went on to find a vaccine for chicken cholera and rabies in both humans and dogs.

xxxxxIncidentally, in 1870 Pasteur studied the manufacture of beer in France and London and, as he had done for the wine industry in the 1860s, came up with a means of preserving the beer over a long period of time. Exporters were thus able to send their product to the Far East and beyond without fear of it deteriorating. ……
xxxxx…… When the Franco-Prussian War broke out in 1870 Pasteur volunteered for military service, but he had suffered a serious paralytic stroke two years earlier and this prevented him from taking part in the fighting. However, as a protest, he returned the honorary medical degree that he had received from the Prussian University of Bonn in 1868!
Vb-1862-1880-Vb-1862-1880-Vb-1862-1880-Vb-1862-1880-Vb-1862-1880-Vb-1862-1880-Vb





 xxxxxIn 1865 the English surgeon Joseph Lister, influenced by Louis Pasteur’s work on bacteria, became the founder of antiseptc medicine. By introducing strict rules of hygiene in the operating theatre and applying carbolic acid, a powerful disinfectant, to reduce the possibility of sepsis (infection) after surgery, he achieved a two-
xxxxxIn 1865 the English surgeon Joseph Lister, influenced by Louis Pasteur’s work on bacteria, became the founder of antiseptc medicine. By introducing strict rules of hygiene in the operating theatre and applying carbolic acid, a powerful disinfectant, to reduce the possibility of sepsis (infection) after surgery, he achieved a two-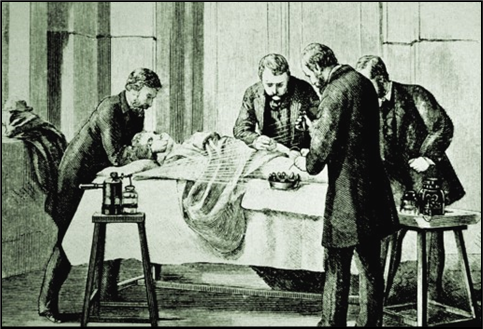 xxxxxIn 1869 Lister was appointed to the chair of Clinical Surgery at Edinburgh, succeeding his former tutor James Syme. He continued his antisepsis work, aided by the advances made in this direction by German surgeons during the Franco-
xxxxxIn 1869 Lister was appointed to the chair of Clinical Surgery at Edinburgh, succeeding his former tutor James Syme. He continued his antisepsis work, aided by the advances made in this direction by German surgeons during the Franco-

 Alphonse Laveran (1845-
Alphonse Laveran (1845-
 xxxxxLouis Pasteur (1822-
xxxxxLouis Pasteur (1822- xxxxxAn opportunity for Pasteur to learn more about infectious diseases came in 1865 when he was the administrator and director of scientific studies at the École Normale in Paris. It was then that he was commissioned by the government to go to the assistance of the silk industry in southern France. A disease among the silkworms, known as pebrine, had killed off the silkworms in large numbers and put this thriving industry in danger of complete collapse. After microscopic observation of the diseased silkworms, the moths and their eggs, Pasteur proved that the disease was due to a tiny parasite and that apart from being highly contagious, the disease was also hereditary. His solution was to destroy all infested worms and mulberry leaves (on which the worms fed) and re-
xxxxxAn opportunity for Pasteur to learn more about infectious diseases came in 1865 when he was the administrator and director of scientific studies at the École Normale in Paris. It was then that he was commissioned by the government to go to the assistance of the silk industry in southern France. A disease among the silkworms, known as pebrine, had killed off the silkworms in large numbers and put this thriving industry in danger of complete collapse. After microscopic observation of the diseased silkworms, the moths and their eggs, Pasteur proved that the disease was due to a tiny parasite and that apart from being highly contagious, the disease was also hereditary. His solution was to destroy all infested worms and mulberry leaves (on which the worms fed) and re-


